DILAPAN-S healthcare economics
Learn how DILAPAN-S incurs significant cost and time savings; A newly published 4-page literature summary of recent RCTs, economic analyses, and case studies demonstrates cost and time savings, with additional savings for outpatient inductions.
Some of the key findings include:
- A saving of 2.4hours of staff time per induction vs. dinoprostone vaginal insert
- DILAPAN-S outpatient ripening incurs additional cost savings of 11%
- 20% higher vaginal delivery rate within 24 hours vs. inpatients
DILAPAN-S outpatient cervical ripening reduces the length of hospital stay and staff time requirements
A randomized trial of outpatient compared with inpatient preinduction cervical ripening using a synthetic osmotic dilator (HOMECARE trial)
Saad AF, Gavara R, Saade G, et al. Outpatient Compared With Inpatient Preinduction Cervical Ripening Using a Synthetic Osmotic Dilator Obstetrics & Gynecology: October 2022;Volume 140 – Issue 4 – p 584-590
OBJECTIVE:
To assess whether outpatient cervical ripening with a synthetic osmotic dilator shortens the length of hospital stay in term pregnancies undergoing labor induction.
METHODS:
Pregnant participants scheduled for labor induction at term with unfavorable cervix (less than 3-cm dilated and less than 60% effaced) and not requiring inpatient maternal or fetal monitoring were consented, and synthetic osmotic dilator rods were inserted on the day of scheduled induction. After reassuring fetal heart tracing, patients randomized to the outpatient group were asked to return 12 hours after insertion or sooner if needed. Those randomized to the inpatient group remained in the hospital. After the first round of ripening, additional ripening, oxytocin, and labor management were left up to the clinical health care professionals. The primary outcome was the proportion of participants with hospital stays longer than 48 hours. We estimated that a sample size of 338 would provide 85% power to detect a 30% difference between groups.
RESULTS:
From November 2018 to November 2021, 339 participants were randomized (171 inpatient, 167 outpatient, one withdrawal). Four patients in the outpatient group were admitted before12 hours for suspected labor and rupture of membranes, and 19 in the inpatient group had the device removed before 12 hours. The proportion of participants with hospital stays longer than 48 hours was lower in the outpatient group compared with the inpatient group (89 [53%] vs 152 [89%], relative risk [RR] 0.60, 95% CI 0.52–0.70). Patients in the outpatient group had a shorter total length of stay and time from admission to active labor. They were more likely to have a vaginal delivery within 24 hours of admission and were less likely to receive analgesics during ripening. Route of delivery and other maternal and neonatal outcomes were not significantly different between groups.
CONCLUSION:
Outpatient cervical ripening with a cervical osmotic dilator decreased hospital stay compared with inpatient ripening, without significant adverse outcomes.
Reduction in staff time requirement by 2.4 hours vs dinoprostone
A cost-consequence analysis based on data from a large randomised trial (SOLVE) and the clinical practice of three UK maternity units.
Walker KF et al. Synthetic osmotic dilators (Dilapan-S) or dinoprostone vaginal insert (Propess) for inpatient induction of labour: A
UK cost-consequence model. Eur J Obstet Gynecol Reprod Biol. 2022 Nov;278:72-76
Objective
To estimate the costs of synthetic osmotic dilators (Dilapan-S) compared to dinoprostone vaginal inserts (Propess) for inpatient induction of labour (IOL).
Study design
A population-level, Markov model-based cost-consequence analysis was developed to compare the impact of using Dilapan-S versus Propess. The time horizon was modelled from admission to birth. The target population was women requiring inpatient IOL from 37 weeks with an unfavourable cervix in the UK. Mean population characteristics reflected those of the SOLVE (NCT03001661) trial. No patient data were included in this analysis. The care pathways and staff workload were modelled using data from the SOLVE trial and clinical experience. Cost and clinical inputs were sourced from the SOLVE trial and peer-reviewed literature. Costs were inflated to 2020 British pounds (GBP, £). Outcomes were reported as an average per woman for total costs and required staff time (minutes) from admission for IOL until birth. The model robustness was assessed using a probabilistic, multivariate sensitivity analysis of 2,000 simulations with results presented as the median (interquartile range, IQR).
Results
Dilapan-S was cost neutral compared to Propess. Midwife and obstetrician times were decreased by 146 min (−11%) and 11 min (−54%), respectively. Sensitivity analysis showed that in 78% of simulations, use of Dilapan-S reduced midwife time with a median of −160 min (IQR −277 to −24 min). Costs were reduced in 54% of simulations (median -£33, IQR -£319 to £282).
Conclusions
The model indicates that adoption of Dilapan-S is likely to be cost-neutral and reduce staff workload in comparison to Propess. Results require support from real-world data and further exploration of Dilapan-S is to be encouraged.
Women undergoing cervical ripening with DILAPAN-S have similar vaginal delivery rate compared to dinoprostone with fewer instances of uterine tachysystole, significantly reduced analgesia need and substantially better maternal satisfaction outcomes.
A randomized trial of synthetic osmotic dilator for induction of labor versus dinoprostone vaginal insert (SOLVE trial)
Gupta JK, Maher A, Stubbs C, et al. A randomized trial of synthetic osmotic cervical dilator for induction of labor vs dinoprostone vaginal insert. Am J Obstet Gynecol MFM. 2022;4:100628.
OBJECTIVE:
To compare the efficacy, maternal and neonatal safety, and maternal satisfaction of a synthetic osmotic cervical dilator (Dilapan-S) with dinoprostone.
STUDY DESIGN
This was an open-label, superiority randomized controlled trial in four English hospitals. Eligible participants were women ≥ 16 years of age undergoing induction of labor for a singleton pregnancy, ≥ 37 weeks’ gestation with vertex presentation and intact membranes. Women were randomly assigned to receive Dilapan-S or dinoprostone using a telephone randomization system minimized by hospital, parity, BMI and maternal age. The induction agent was replaced as required until the cervix was assessed as favorable for labor by Bishop score. The primary outcome was failure to achieve vaginal delivery (i.e. Cesarean delivery). Secondary outcome measures included maternal and neonatal adverse events. Analysis was by intention-to-treat, adjusting for design variables where possible.
RESULTS
Between 19 December 2017 and 26 January 2021, 674 women were randomized (337 to Dilapan-S and 337 to dinoprostone). The trial did not reach its planned sample size of 860 due to restrictions on research during the Covid-19 pandemic.
The primary outcome was missing for two women in the dinoprostone group. Failure to achieve vaginal delivery (Cesarean section) occurred in 126 women (37.4%) allocated to Dilapan-S, and 115 (34.3%) women allocated to dinoprostone (adjusted risk difference 0.02, 95% confidence interval -0.05 to 0.10). There were similar maternal and neonatal adverse events between the groups.
CONCLUSION
Women undergoing induction of labor with Dilapan-S have similar rates of caesarean section and maternal and neonatal adverse events compared to dinoprostone.
DILAPAN-S is comparable to low-dose oral misoprostol in vaginal delivery within 24 hours, while offering safety benefits and superior maternal satisfaction.
A randomized trial of synthetic osmotic dilator for induction of labor versus low-dose oral misoprostol (COMRED trial)
Gavara R, Saad AF, Wapner RJ, et al. Cervical Ripening Efficacy of Synthetic Osmotic Cervical Dilator Compared With Oral Misoprostol at Term: A Randomized Controlled Trial. Obstetrics & Gynecology. 2022;139(6):1083-1091. doi:10.1097/aog.0000000000004799
OBJECTIVE:
To evaluate whether a synthetic osmotic cervical dilator is noninferior to oral misoprostol for cervical ripening.
METHODS:
In an open-label, noninferiority randomized trial, pregnant women undergoing induction of labor at 37 weeks of gestation or more with Bishop scores less than 6 were randomized to either mechanical cervical dilation or oral misoprostol. Participants in the mechanical dilation group underwent insertion of synthetic osmotic cervical dilator rods, and those in the misoprostol group received up to six doses of 25 micrograms orally every 2 hours. After 12 hours of ripening, oxytocin was initiated, with artificial rupture of membranes. Management of labor was at the physician’s discretion. The primary outcome was the proportion of women achieving vaginal delivery within 36 hours of initiation of study intervention. Secondary outcomes included increase in Bishop score, mode of delivery, induction to delivery interval, total length of hospital stay, and patient satisfaction. On the basis of a noninferiority margin of 10%, an expected primary outcome frequency of 65% for misoprostol and 71% for mechanical methods, and 85% power, a sample size of 306 participants was needed.
RESULTS:
From November 2018 through January 2021, 307 women were randomized, with 151 evaluable participants in the synthetic osmotic cervical dilator group and 152 in the misoprostol group (there were four early withdrawals). The proportion of women achieving vaginal delivery within 36 hours was higher with mechanical cervical dilation compared with misoprostol (61.6% vs 59.2%), with an absolute difference of 2.4% (95% CI 29% to 13%), indicating noninferiority for the prespecified margin. No differences were noted in the mode of delivery. Tachysystole was more frequent in the misoprostol group (70 [46.4%] vs 35 [23.3%]; P5.01). Participants in the synthetic osmotic cervical dilator group reported better sleep, less unpleasant abdominal sensations, and lower pain scores (P,.05).
CONCLUSION: Synthetic osmotic cervical dilator is noninferior to oral misoprostol for cervical ripening. Advantages of synthetic osmotic cervical dilator include a better safety profile and patient satisfaction, less tachysystole, lower pain scores, and U.S. Food and Drug Administration approval.
With 81 % of vaginal delivery rate DILAPAN-S represents a highly effective cervical ripening agent. Trial indicated a trend towards a potentially lower caesarean section rate in DILAPAN-S group vs Foley balloon. DILAPAN-S was evaluated as superior in maternal satisfaction.
A randomized controlled trial of DILAPAN-S vs Foley balloon for preinduction cervical ripening (DILAFOL trial)
Saad AF, Villarreal J, Eid J, et al. A randomized controlled trial of Dilapan-S vs Foley balloon for preinduction cervical ripening (DILAFOL trial). Am J Obstet Gynecol. 2019;220:275.e1-9.
OBJECTIVE:
The objective of the study was to test the hypothesis that Dilapan-S is not inferior to the Foley balloon for preinduction cervical ripening at term.
STUDY DESIGN:
Pregnant women ≥37 weeks scheduled for induction with unfavorable cervix (≤3 cm dilated and ≤60% effaced) were randomly assigned to 12 hours of either Foley balloon inflated with 60 mL saline or Dilapan-S for cervical ripening. If the cervix remained unfavorable, then 1 more round of the assigned dilator was used. Management following ripening was left up to the clinical providers. The primary outcome was vaginal delivery. A satisfaction survey was also obtained after the preinduction period. Sample size was based on a noninferiority margin of 10%, 90% power, and an estimated frequency of vaginal delivery of 71% in Foley balloon and 76% in Dilapan-S.
RESULTS:
From November 2016 through February 2018, 419 women were randomized (209 to Foley balloon; 210 to Dilapan-S). In the intent-to-treat analysis, vaginal delivery was more common in Dilapan-S vs Foley balloon (81.3% vs 76.1%), with an absolute difference with respect to the Foley balloon of 5.2% (95% confidence interval, -2.7% to 13.0%) indicating noninferiority for the prespecified margin. The difference was not large enough to show superiority. Noninferiority was confirmed in the per-protocol population (n = 204 in the Foley balloon, n = 188 in Dilapan-S), supporting the robustness of the results. Secondary outcomes were not different between groups, except for a longer time the device remained in place in Dilapan-S compared with the Foley balloon. Maternal and neonatal adverse events were not significantly different between groups. A priori interaction analyses showed no difference in the effect on vaginal delivery by cervical dilation at randomization, parity, or body mass index >30 kg/m2. Patients with Dilapan-S were more satisfied than patients with the Foley balloon as far as sleep (P = .01), relaxing time (P = .001), and performance of desired daily activities (P = .001).
CONCLUSION:
Dilapan-S is not inferior to the Foley balloon for preinduction cervical ripening at term. Advantages of Dilapan-S over Foley include Food and Drug Administration approval, safe profile, no protrusion from the introitus, no need to keep under tension, and better patient satisfaction.
Consistent Bishop score gain (+3,6) across all types of induced women
An international multicentre observational study of Dilapan-S in labour induction
Gupta J. et al. Synthetic osmotic dilators in the induction of labour – An international multicentre observational study, Eur J Obstet Gynecol Reprod Biol, 2018 Oct;229:70-75.doi: 10.1016/j.ejogrb.2018. 8.004. Epub 2018 Aug 3.
INTRODUCTION
To evaluate the effects of synthetic osmotic dilators (Dilapan-S/ Dilasoft) in women who required induction of labour in a large prospective multicentre international observational study.
MATERIALS AND METHODS
Primary outcomes were duration of Dilapan-S/Dilasoft insertion (hours), total induction – delivery interval (hours) and the rate of vaginal deliveries within 24 h (%). Secondary outcomes were the number of dilators inserted, Bishop score increase after extraction of Dilapan-S/Dilasoft, complications during induction (uterine contractions, uterine tachysystole and hyperstimulation, effect on the fetus) and post induction (infections and neonatal outcomes), agents / procedures used for subsequent induction of labour, immediate rate of spontaneous labours following cervical ripening period, rate of spontaneous vaginal deliveries, rate of instrumental vaginal deliveries and caesarean sections.
RESULTS
Total of 543 women were recruited across 11 study sites, of which, 444 women were eligible for analysis. With Dilapan-S/Dilasoft use of <12 h (n = 188) the overall vaginal delivery rate was 76.6% with 45.7% of these births occurring within 24 h, 66% within 36 h and 75.5% within 48 h from insertion of Dilapan-S/Dilasoft. The mean insertion-delivery interval for this group was 24.3(±10.4) hours. With Dilapan-S/Dilasoft use of >12 h (n = 256), the overall vaginal delivery rate was 64.8%, with 16% of these births occurring within 24 h, 48.4% within 36 h and 54.7% within 48 h from insertion of Dilapan-S/Dilasoft. The mean insertion-delivery interval for this group was 39.1(±29.2) hours. The mean gain in the Bishops score was +3.6(±2.3). The mean number of Dilapan-S/Dilasoft dilators used was 3.8 (±1.1). The overall rate of caesarean section was 30.1%. The overall complication rate was low including infection risk. No adverse neonatal outcome was attributable to the use of Dilapan-S/Dilasoft.
CONCLUSION
Dilapan-S/Dilasoft are safe and effective methods for cervical ripening. Their use is associated with low maternal and neonatal complication rates. Future research should aim at level I clinical trials comparing Dilapan-S to other mechanical or pharmacological cervical ripening agents.
With the caesarean section rate rising, trial of labour after caesarean (TOLAC) appears as a viable option to counteract this trend. 52% chance to experience vaginal birth following previous caesarean section may lessen women‘s misgiving that subsequent delivery is likely to finish with the caesarean section again.
A prospective dual centre study comparing synthetic osmotic dilator vs. prostaglandin E2
Koenigbauer J. et al. Cervical ripening after cesarean section: a prospective dual center study comparing a mechanical osmotic dilator vs. prostaglandin E2, J Perinat Med 2;49(7):797-805. Sept 2021
OBJECTIVES
Worldwide, the overall cesarean section is rising. Trial of labor after cesarean (TOLAC) is an overall safe option with an immediate impact on neonatal and maternal short- and long-term health. Since the use of prostaglandins in cervical ripening is associated with an increased risk of uterine rupture, mechanical methods as balloon catheters or osmotic dilators have been suggested for cervical ripening prior to induction of labour. Here we are analyzing and comparing the VBAC rate, as well as maternal and fetal outcome in cervical ripening prior to TOLAC.
METHODS
This prospective dual center study analyses maternal and neonatal outcomes of TOLAC in women with an unfavorable cervix requiring cervical ripening agent. The prospective application of an osmotic dilator (Dilapan-S, n=104) was analysed in comparison to the retrospective application of off-label dinoprostone (n=102).
RESULTS
The overall fetal and neonatal outcome revealed no significant differences in both groups. Patients receiving cervical ripening with the osmotic dilator delivered vaginally/by ventouse in 52% of cases, compared to 53% when using dinoprostone (p=0.603). The interval between application to onset of labor was significantly higher in the osmotic dilator group (37.9 vs.20.7 h, p=<0.001). However, time from onset of labor to delivery was similar in both groups (7.93 vs. 7.44 h, p=0.758). There was one case of uterine rupture in the dinoprostone group.
CONCLUSIONS
Our data shows that the application of the osmotic dilator leads to similar outcomes in VBAC rate and time from onset of labor to delivery as well as safety in both groups compared to off-label use dinoprostone. Cervical ripening using the mechanical dilator is a viable and effective option, without the risk of uterine hyperstimulation.
Predictable and reliable mode of action due to its synthetic origin.
An experimental in vitro study comparing natural and synthetic osmotic dilators in selected parameters influencing their clinical efficacy.
Drunecký T. et al. Experimental comparison of properties of natural and synthetic osmotic dilators, Archives of Gynecology and Obstetrics volume 292, 349–354 (2015)
PURPOSE
To compare natural and synthetic osmotic dilators in selected parameters influencing their clinical efficacy.
METHODS
Diameters of Laminaria and synthetic dilators (Dilapan-S and Dilasoft) were measured in dry state, during free swelling in isotonic solution and during swelling against a force. Three aspects were evaluated-diameter increase, speed of action and consistency of action.
RESULTS
The maximum diameter increase of 3 and 4-mm Dilapan-S was 3.6 and 3.3 times, of Dilasoft 3.2 and 3.1 times, respectively. For Laminaria, it was 2.9 and 2.7 times. The difference between synthetic dilators and Laminaria was statistically significant (p < 0.01). Synthetic dilators also swelled faster. Under applied counter force, synthetic dilators increased their diameter more than Laminaria (+3.6 mm for Dilapan-S, +3.8 mm for Dilasoft, +1.2 mm for Laminaria; p < 0.01) and achieved faster expansion. Synthetic dilators also showed significantly higher consistency between samples in all experiments.
CONCLUSIONS
Synthetic dilators compared to Laminaria reached higher maximum diameters, acted faster, were more consistent and were able to expand against force three times more. The results support clinical observations that synthetic dilators are more suitable and preferable for same-day D&E procedure and that fewer synthetic dilators are needed to achieve the same effect.
DILAPAN-S in numbers
years of experience on the market

countries we work in
of vaginal deliveries

Consistently superior maternal satisfaction accross multiple clinical trials
Brochure for clinicians
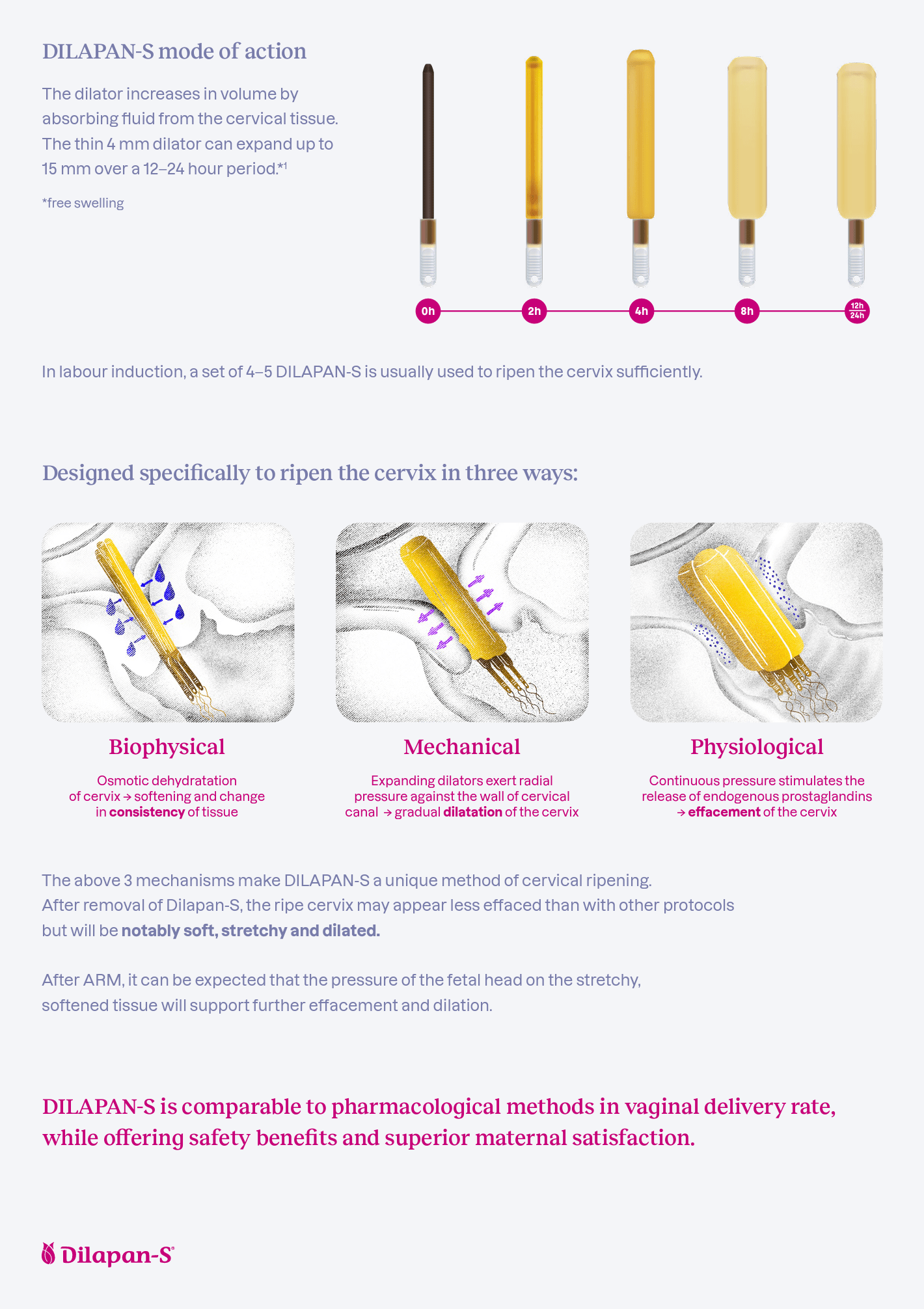
Non-pharma cervical ripening with DILAPAN-S is perfectly suited for outpatient regimen as it does not encourage contractions and contains no pharmacological agents.
Any further information required?